Rhino-orbito-cerebral mucormycosis causing cranial nerve abscess in post - Covid-19 status.
DESCRIPTION
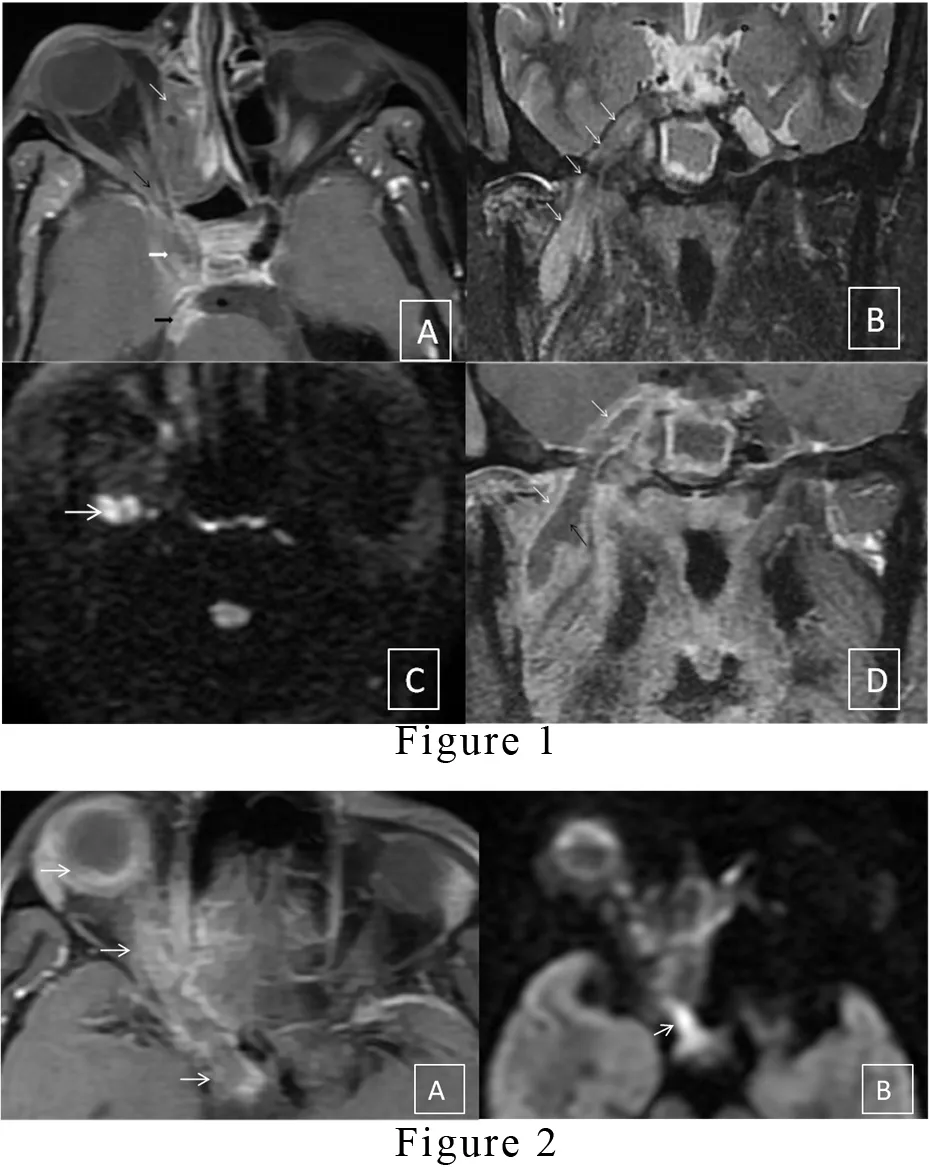
Perineural extension of fungal infection is a rare complication observed in post-Covid-19 immunocompetent mucormycosis patients during this pandemic. Rhino-orbito-cerebral mucormycosis is an opportunistic fungal infection caused by members of family mucoraceae. Mucormycosis proved to be the lethal disease in untreated diabetic or patients on immunosuppressive therapy with the same pattern of spread and severity. [1,2] Rhino-orbito-cerebral mucormycosis has been declared endemic by the Indian government recently. Due to the aggressive pattern of spreading in this disease, it rapidly involves the surrounding structures. Cerebral extension of the organism occurs either by direct extension, hematogenous route or perineural spread. Over two months, we have observed nine patients with perineural spread involving cranial nerves during this endemic. The peculiar imaging findings in a perineural spread include thickened nerves with abnormal enhancement and perineural fat stranding. Initially, the enhancement in the affected nerve represents neuritis. However, it can progress into a full-blown abscess. The trigeminal nerve is a large cranial nerve with a unique course that enables us to easily demonstrate this evolution line. Magnetic resonance imaging (MRI) stands to be the best diagnostic and non-invasive imaging technology that produces three-dimensional detailed anatomical images that help determine disease spreading with treatment.[1] This article highlights the role of MRI in the diagnosis of perineural complications observed in rhino-orbito-cerebral mucormycosis. Here, we present two representative cases of a 55-year-old female and a 60-year-old male who presented to our hospital with facial pain, facial numbness and high-grade fever. On initial examination, periorbital soft tissue swelling and facial redness were found with a history of hospitalization for Covid-19 pneumonitis in the recent past. The patients were administered steroids during the previous hospital stay. On relevant laboratory investigations, both the patients had deranged blood glucose levels. The patients underwent an MRI of paranasal sinuses and brain, revealing orbital cellulitis, pansinusitis, abnormal signals in the premaxillary skin, retro-antral fat and masticator space extending to the right cavernous sinus [Figure1 A]. The inferior turbinates and paranasal sinuses also had non-enhancing areas on post-contrast MRI, representing necrosis. In the first patient, the mandibular division of the right trigeminal nerve was thickened and showed heterogeneous signals on all MRI sequences [Figure 1B]. The Diffusion-weighted image (DWI) image shows diffusion restriction in the abscess in the nerve [Figure 1C]. On post-contrast, T1 fat-suppressed images, the nerve reveals peripheral enhancement with central liquefied non enhancing collection, represent an abscess [Figure 1D]. In another similar patient, there is the involvement of the pre septal soft tissue, eye globe and optic nerve up to the optic chiasma on the right side was observed[Figure 2A], and the path of spread is seen extending along the optic nerve on a diffusion-weighted image[Figure 2B]. There are very few documented cases available in the literature describing the perineural spread of fungal infection, especially after this Covid era; however, similar cases have been reported previously in uncontrolled diabetic patients by Bruno Galletti et al.[1] A surgical biopsy from the inferior turbinate was done, which revealed non-septate fungal hyphae. Both the patients managed with anti-fungal drugs; however, they did not improve much. Both the patients are receiving treatment in our hospital till the writing of this article.
LEARNING POINTS
-
An emergency CT scan should be performed to access invasive rhino-sinusitis in immune-suppressed or uncontrolled diabetic patients presenting with symptoms limited to paranasal sinuses. If there is a suspicion of CNS or orbital involvement, MRI stands to be the ideal imaging modality.
-
If any of these modalities raises suspicion for Rhino-orbito-cerebral mucormycosis, immediate biopsy and anti-fungal treatment must be started. Even if the first biopsy comes negative for fungal elements and imaging shows typical findings, the condition should still be treated as invasive fungal sinusitis, and a second biopsy should be performed.
-
Nerve abscess is an extremely uncommon entity, can only be diagnosed if the radiologist is familiar with the pathology and has a high suspicion. MRI is the ideal diagnostic tool for this pathology that also helps in accessing the disease progression.
REFERENCES
-
Galletti B, Freni F, Meduri A, Oliverio GW, Signorino GA, Perroni P, Galletti C, Aragona P, Galletti F. Rhino-Orbito-Cerebral Mucormycosis in Diabetic Disease Mucormycosis in Diabetic Disease. J Craniofac Surg. 2020 Jun;31(4) e321-e324. doi:10.1097/scs.0000000000006191.
-
Anselmo-Lima WT, Lopes RP, Valera FC, Demarco RC. Invasive fungal rhinosinusitis in immunocompromised patients. Rhinology. 2004 Sep;42(3):141-4. PMID: 15521667.
LEGENDS:
-
Figure 1: (A) T1 weighted fat-saturated (T1W FS) post-contrast, axial image show shows Heterogenous enhancement in the right ethmoid sinus (white arrow), orbital apex (black arrow), extending to right cavernous sinus (thick white arrow) and then till fifth nerve nucleus (thick black arrow). (B) Short tau inversion recovery (STIR) image in the coronal plane shows Abnormally increased signals along the right mandibular nerve (white arrows). (C) Diffusion-weighted image (DWI) in the axial plane depicts restricted diffusion in the mandibular nerve (white arrow). (D)T1 weighted fat, saturated post-contrast image in coronal plane demonstrates Peripheral enhancement (white arrows) with central liquefied non-enhancing collection (black arrow) along mandibular nerve passing through foramen ovale.
-
Figure 2: (A) T1 weighted fat-saturated (T1W FS) post-contrast, axial image show contiguous involvement of the pre septal soft tissue, eye globe and optic nerve up to the optic chiasma on the right side (white arrow). (B)The path of spread can also be evaluated on a diffusion-weighted image(White arrow).