Sturge-Weber syndrome: An unusual adult age group presentation.
DESCRIPTION
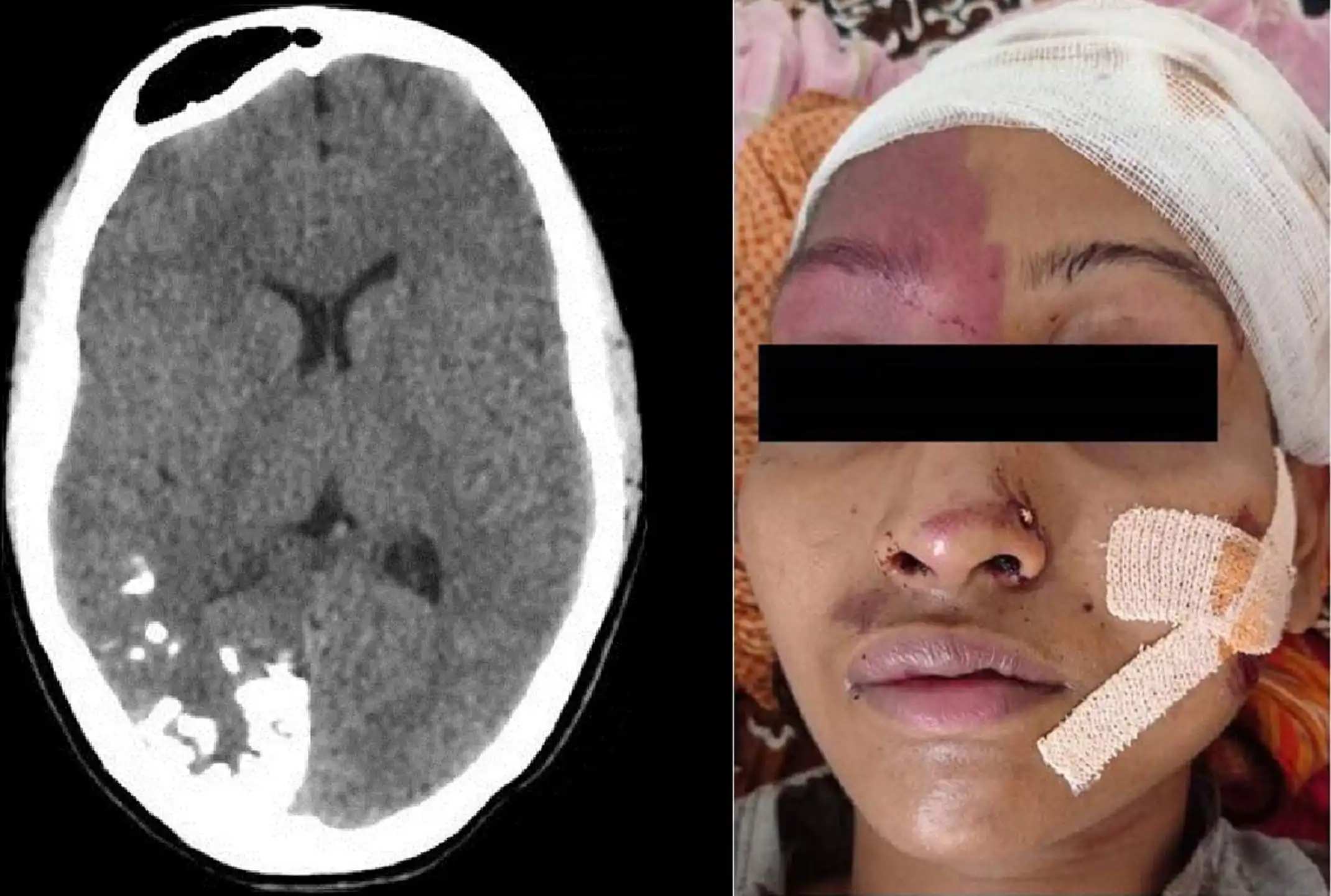
Sturge-Weber syndrome is an unusual neurocutaneous syndrome that includes a facial port- wine stain and leptomeningeal angiomatosis (1,2). Weber described the characteristic gyriform intracranial calcifications (3), which are located in the cortex underlying the leptomeningeal vascular malformations that rarely appear before two years of age. Clinical presentation may be because of congenital facial cutaneous hemangioma, focal neurological deficit seizures, glaucoma to incidental findings. Based on classical features, it is divided into three main types, i.e. Type I is a classic syndrome with both facial and leptomeningeal angiomas, Type II is facial angioma without evidence of intracranial disease, and Type III is isolated leptomeningeal angioma. A 20-year-old girl presented to the emergency room with a large scalp hematoma post-road-traffic accident. On physical examination, she had an accelerated pulse rate of 100 per minute; otherwise, the rests of the vitals were normal. After providing emergency care for her scalp and face wounds, she was referred for computed tomography (CT) scan of the head. The CT scan revealed a tram-track pattern of calcification in the brain's right occipital and temporal lobes (Figure 1). The right cerebral hemisphere was atrophied to a milder grade with a prominence of ipsilateral paranasal sinuses. The choroid plexus in the right lateral ventricle appeared bulky as compared with the normal counterpart on the left side. She also had a large subgaleal hematoma over her scalp. After reviewing the CT scan, the previous history of any seizures or neurological deficit was asked, which was negative. On re-examining her face, a port-wine stain was observed around her right eye and forehead (Figure 2). A diagnosis of Sturge- Weber syndrome (Type 1) was made, and she was kept on follow-up. Surprisingly, she remains asymptomatic till 20 years of age, and the diagnosis is made on a non-related hospital visit. Etiologies for calcifications within the brain parenchyma or vasculature can be classified into several major categories: physiologic/age-related, dystrophic, congenital disorders/phakomatoses, infectious, vascular(like stroke sequelae, arteriovenous malformation), neoplastic, metabolic/endocrine, inflammatory and toxic diseases. In this particular case, the typical tram- rack appearance raised the suspicion and prompted the re- assessment for any facial stain. Ultimately, the diagnosis of the Sturge-Weber syndrome could be reached. This tram-track pattern of cortical calcifications results from leptomeningeal vascular malformations found in patients with Sturge-Weber syndrome. A theory suggests that the primary defect for this entity occurs during the lamination phase of embryological development when there is a normal connection between the developing cortical veins and the superior sagittal sinus. Suppose this communication is not maintained during the differentiation and separation of these two circulations, the venous outflow effects, leading metabolic insufficiency to that part. The cerebral cortex underlying the areas of this leptomeningeal vascular malformation usually becomes atrophic, dysfunctional and calcified. (4) Calcification can be more extensive and usually observed in areas of cortical atrophy. Ocular involvement can occur, including buphthalmos and scleral or choroidal angiomas, choroidal detachment and subacute haemorrhage. (1) Choroid plexus enlargement, ipsilateral calvarial thickening and dilatation of the paranasal sinuses are the other features that can be observed on imaging.
LEARNING POINTS
-
Sturge-Weber syndrome is a sporadic neurocutaneous syndrome. Imaging features in patients presenting with facial angioma are classic with or without symptoms.
-
Intracranial calcifications are common findings, and NCCT is the modality of choice to characterize calcifications.
-
Cortical calcification may or may not have to present symptoms; therefore, the patient's age, clinical findings, location, the pattern of intracranial calcifications and presence of any cutaneous lesion are essential clues for the proper diagnosis and management.
LEGENDS:
-
Boyer RS. Disorders of histogenesis: neurocutaneous syndromes. In: Osborn AG, ed. Diagnostic neuroradiology. St Louis, Mo: Mosby, 1994; 72–113.
-
Case 119. In: Fischebein NJ, Dillon WP, Barkovich AJ, eds. Teaching atlas of brain imaging. New York: Thieme, 2000; 461–464.
-
Weber FP. Right-sided hemi-hypertrophy resulting from right-sided congenital spastic hemiplegia, with a morbid condition of the left side of the brain, revealed by radiograms. J NeurolPsychopathol 1922; 3:134–139.
-
Smirniotopoulos JG, Murphy FM. The phakomatoses. AJNR Am J Neuroradiol 1992; 13:725–7461.